The fungus between the toes is a disease that is very easy to absorb.But getting rid of him is anything but so easy.The disease can take years, often a bacterial infection is followed.When the first symptoms occur, it is very important to contact a dermatologist and not to convey yourself.
Why does the fungus develop between the toes?
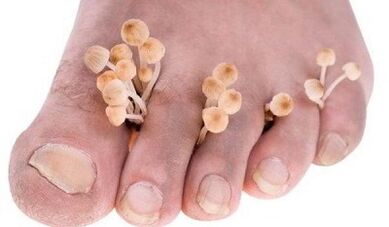
The fungus between the toes is the most common type of fungal infection that occurs in 70% of the population of our planet.This disease is especially in people who are constantly in a damp or hot environment and often sweat due to high physical exertion.This includes banners, swimmers, employees of hot workshops, etc. Children are much less common (no more than 4%), but incidence increases dramatically in adolescence.
The disease is caused by various types by dermatophil mushrooms: Red Trichophyton, Interdaltsev -Trichophyton and some types of epidermophytons.All of these pathogens are characterized by a high degree of survival in the environment.You can hold in shoes for a long time on the floors in the bath house and in the sauna, bathing equipment, linen.
You can infect the beach less often in a bath, a sauna, a pool.Therefore, it is so important to observe the hygiene rules: Use just an individual towel, do not contact you in public places barefoot and use individual shoes.
On the surface of the body, mushrooms produce enzymes (keratinase), break down the keratin - the protein of the surface lifts.This can penetrate an infection into the epidermis and multiply there.Mushroom cell membranes contain substances (manners) that can inhibit local immunity.Manins also suppress the reproduction of the surface cells of the epidermis, which disrupts their switching off and cleaning, which leads to a longer and chronic course of the disease.
Factors that contribute to the spread and implementation of fungus
Such factors include:
- Shoes that press the legs that violate blood circulation and do not air;
- Do sports and serious physical work;
- Trauma of the feet with a skin injury;
- Increased immunity, for example, against the background of diabetes, longer administration of certain medicines (glucocorticoid hormones), HIV infection;
- Violation of blood circulation in the feet of the feet against the background of the atherosclerosis of the lower extremities, flat feet and so on.
If a person has a normal general and local immunity, the fungus cannot be able to overcome the protective barrier of the skin and infiltrate the skin.All factors that suppress the skin tamunity make it possible to introduce pathogenic mushrooms into the epidermis without an obstacle, which leads to a pathological process.
Symptoms of an infection
When introducing pathogenic mushrooms into the skin, areas with thin and sensitive skin are mainly influenced by interdigital gaps.This is where the infection begins, which can then spread over the entire foot.The first thing an infected person experiences is to itch and burn between the toes.
Itching can be very strong or insignificant or even completely missing and only occur against the background of the sweating of the feet or a decrease in immunity.Significant itching, drought, painful cracks in interdigital rooms contribute to the addition of a bacterial infection and the development of purulent processes.
Sometimes sluggish bubbles occur between the fingers, filled with transparent liquid that open up quickly and form erosion.And this type of illness can be complicated by adding a bacterial infection.
The most characteristic for the hidden course of the mushroom between the toes, which is characterized by regular itching.Often such patients do not suspect the presence of infections and spread them, among other things.
How the disease flows
The fungus can manifest itself in different ways.The following forms of the disease are differentiated:

- Intrigal- most frequently;It manifests itself in the form of itching and burning between the toes, drought, tearing with the release of the lug and the subsequent development of maceration (loosening of the skin under the influence of the liquid);Inflammation often goes to the plantar surface of the feet and almost never backwards.Bacterial infections often combine;
- Dyshidrotic.
- deleted- flows unnoticed;Occasionally there is a slight itching;A moderate thin peeling occurs between the toes (mostly between 1 and 2 or 5), very small and unnoticed by the patients with cracks.
The fungus in interdigital gaps can occur as an independent disease or is a manifestation of a general infection.The fungus often changes to nail plates with the development of onychomycosis.Sometimes there is a combined lesion of the skin of the feet and skin in the area of large wrinkles on the body and hands.In the latter case, the infection often develops according to the principle of "two foot - a brush".
How to identify an infection
The diagnosis is carried out on the basis of an examination of a dermatologist and is confirmed by laboratory research:
- The microscopy method- The skin elements (scales) taken from the lesion are examined under a microscope;This is the most common method.You can identify a fungal infection, but cannot determine the type of fungus.
- Microbiological examination- sowing biological materials that were taken from the lesion on nutrient media;Soil mushrooms are easy to identify, but do not always lend growth of the laboratory conditions.Therefore, it often remains to concentrate on the microscopy method.
The basic principles of treatment
Antimyotika are used to treat interdigital gaps.If the disease does not run long, progress, external means are used.In the case of severe fungal infections with the tendency to spread or develop microbial eczema, antifungals of the general (system) effect are used.
The external use of antifungals requires preliminary preparation.Pathologically modified skin elements are removed from the skin surface: peeling, destroying places and the remains of bursting bubbles.If possible, they try to relieve inflammation and swelling of tissues.
Create the following procedures:
- If there is a pronounced inflammation and swelling of the tissue, lotions with 2% solutions from boric acid, special ointments, are prescribed.If it doesn't help, corticosteroid ointments are prescribed in short courses.
- In the presence of scales and crusts, the affected areas of the body surface are lubricated twice a day with salicyl era jelly, and then swimming pools are carried out with a 2% soda solution.
The main treatment is only carried out after cleaning.If there is a suspicion of mixed mushroom bacterial infections, combined ointments are used, including antifungal, antibacterial and anti -allergic components.
Pharmaceutical therapy
The most modern drugs for the treatment of such diseases are medication whose active substance is terbinafin, which is part of the external utility products that are produced by various pharmaceutical companies under their trade names.These are 1% creams, gels, sprays and solutions for external use.
This substance occurs slightly into the epidermis.His concentration is enough to suppress the important activity of the infection 4 hours after using his concentration.The concentration of the product gradually gathers in the skin and after therapy is many times higher than the concentration causing the death of mushrooms.In addition, it does not penetrate the middle and deep layers of the skin and does not systemically affect the body.A characteristic of the antifungal is that it has an antibacterial effect that suppresses the vital activity of most pathogenic bacteria.An additional antibacterial therapy is therefore not always required for the treatment of a fungal-bacterial infection.
Carn, spray and gel are applied to pathologically modified areas of the feet for 7 days.Usually this is enough to completely go through all symptoms of an infection.If necessary, a dermatologist can extend the course of treatment.
With the ineffectiveness of external treatment and the most common, frequently recurring forms of the disease, antifungals are prescribed for the general effect.
With the development of microbial eczema, complex treatment is prescribed, including antifungals, antibiotics and desensitizing active ingredients that reduce allergic moods, inflammation and edema of tissues.In severe allergic and inflammatory processes, glucocorticoid hormones are included in the complex treatment.
People's funds against the interdalcial mushroom
People's funds can also be effective if they are used correctly.Traditional medicine recommends that preparatory treatment for cleaning pathologically modified areas of the feet surface before the start of the antifungals.Cleaning takes place in the same way as before drug treatment.Fixed assets are then used to suppress the vital functions of mushrooms.
- Method 1.Do two to 2 to 3 weeks twice a day for the legs for the legs with a Celandine infusion of a large one (a third of a glass with a crushed grass per liter of boiling water) and then smear the dried surface of the feet with 10% tincture from propolis.
- Method 2.Add 20 ml of ammonia to a glass of water, moisten the bandage, first wrap your fingers and then the whole foot (don't pull yourself tight!) And let it dry.The duration of treatment is 14 days.
- Method 3.Foot baths with vinegar (for 2 liters of water - 100 ml of table vinegar).They are kept a day 14 days before going to bed.After the procedure, dry your legs and slightly sprinkle them with boric acid.
- Method 4.Necessary bathrooms with a touch of waves (20 g MaHorka Pro 1L boiling water, existed for 3 - 4 hours in a thermos box office).Daily before going to bed four weeks before going to bed.After the procedure, the legs have to dry themselves.Wash your feet with water in the morning.
- Method 5.Wash your feet with house soap and wash thoroughly between your fingers.Dry your legs and grease the skin with Celandin juice.Do this every day for 14 days.
- Method 6.Daily legs for legs with 2% soda solution.After the bathroom, dry your legs with a towel fountain and grease with garlic oil.In the morning, wash them with soap.Garlic oil: Mix a teaspoon with a crushed garlic made of 100 g butter until a homogeneous mass is obtained.
- Method 7.Take an equal amount of apple cider vinegar and freshly squeezed carrot juice.Apply the resulting mixture to the affected areas of the skin of the feet several times a day.
How to warn the infection
To prevent the disease, they need:
- Wear rubber slate in a bath, a sauna, the pool, on the beach;
- Never wear someone else's shoes, do not use a towel and bathing accessories from another.
- In the warm season, put on shoes or sandals from light natural materials that run air and absorb moisture.
- Use only individual or disposable tools to carry out a pedicure.
To prevent the RE infection, should:
- Treat the inner surface of the shoes with disinfectable solutions, e.g.B. formalin solutions or vinegar essence;Two days after such processing, the death of all infectious pathogens occurs.
The fungus between the toes is well suited for therapy with modern antifungals and folk methods.However, it is very important to make all efforts in such a way that there is no RE function, including your own shoes and other personal everyday objects.

















